Understanding the New Cervical Cancer Screening Guidelines
Cervical cancer screening has been one of the most impactful public health achievements of the past century. Regular screening with Pap tests and human papillomavirus (HPV) testing has dramatically reduced both the incidence of cervical cancer and deaths from the disease. Recently, the U.S. Department of Health and Human Services updated national cervical screening guidelines to reflect new evidence and technologies — changes that matter for both patients and caregivers.
What’s Changed in the Guidelines?
The updated guidelines expand screening options and clarify who benefits most from each approach:
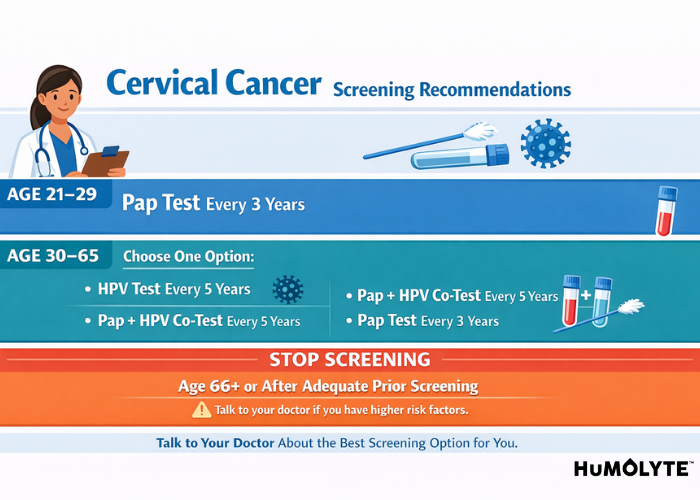
Women aged 21–29: Continue to receive Pap tests (cervical cytology) every 3 years.
Women aged 30–65: Now have more choices:
Primary high-risk HPV testing every 5 years (preferred when available),
Combined Pap and HPV co-testing every 5 years, or
Pap test alone every 3 years if HPV testing isn’t available.
These changes emphasize HPV testing — which detects the virus that causes most cervical cancers — as a primary strategy for preventing invasive cancer. The option for self-collected HPV testing (in some settings) is also included, offering improved accessibility for people who face barriers to clinic-based screening.
Why These Updates Matter
For many patients, especially those without regular access to care, self-collection testing can remove logistical and emotional barriers that keep people from being screened. Expanded screening options also help clinicians tailor care based on individual risk and preferences.
Regular screening matters because cervical cancer can develop silently over years, and early abnormalities are often highly treatable. Detecting HPV or precancerous changes early greatly increases the chances of preventing cancer before it starts.
Who Should Be Screened?
The guidelines apply to people at average risk of cervical cancer — meaning they are not known to have a weakened immune system (such as from HIV), a history of cervical cancer, or other specific risk factors.
Not recommended: Screening more often than advised (“overscreening”),
Important: People with unusual symptoms such as abnormal bleeding should seek evaluation regardless of schedule,
Tailored care: Those with prior cervical disease or higher risk may need individualized screening plans discussed with their clinician.
What Caregivers Should Know
If you’re supporting someone through preventive care, these updates may affect decisions about scheduling screening appointments:
Ask about HPV testing availability. Some clinics offer HPV testing as a first-line option.
Help with navigation. Newer options like self-collection may require guidance on proper use and interpretation.
Insurance coverage matters. Under federal preventive care rules, recommended screening services are generally covered without cost sharing when delivered according to guidelines. J
Final Thoughts
These updated cervical cancer screening guidelines reflect evolving science and aim to reduce barriers to early detection. By expanding options — especially around HPV testing — the goal is to catch disease earlier and prevent cancer more effectively.
Caregivers can play a vital role by helping patients understand their screening choices, recognize the importance of regular prevention, and navigate the healthcare system — especially in communities with historically lower screening rates.
Reference
New Cervical Cancer Screening Guidelines From the US Department of Health and Human Services